Background
What is a Food Allergy?
A food allergy occurs when the body mistakes a specific food as harmful. This leads the immune system to overreact and results in reactions which can range from mild to severe. Remember, the immune system’s job is to protect the body by identifying potential threats and fighting them off. In most cases, the immune system does a good job in identifying true threats. For a child with allergies, however, the immune system mistakenly identifies an otherwise safe ingredient as a threat.
There are two phases in the development of a food allergy:
Sensitization refers to an event: the first encounter with an allergen. This is when the immune system mistakenly identifies the allergen as a threat and creates immunoglobulin E (IgE) antibodies in response. These IgE antibodies are then ready to respond when the body next encounters the allergen. While there are no symptoms at the sensitization phase, your child’s immune system is actively preparing for the next encounter.
Reaction refers to what happens to the body during the later encounters with the allergen. When this happens, the IgE antibodies are already created and ready to respond to the perceived threat. Upon encountering the allergen, the IgE antibodies activate allergy cells called mast cells, which in turn sets off a chain reaction of symptoms in the body.
We find it helpful to think of the reaction phase like a kid’s birthday party:
- The IgE antibodies are like the kids at the party — already sensitized and eager to play.
- The mast cell is like a piñata, hanging in the middle of the room. It's packed full of chemicals, including histamine, but for most of the party, the kids barely notice it.
- The allergen is like the piñata stick.

Introducing the allergen to the body is like introducing a stick to the party. When they see the stick, the kids swarm around it and start hitting the piñata. Eventually, the piñata breaks, releasing candy everywhere and causing exuberant chaos in the room. Similarly, in an allergic child’s body, activating the mast cell sets off a chain reaction throughout the body, leading to hives, swelling, stomach aches, coughing, or more serious symptoms.
It’s helpful to remember that allergic reactions to food are the exception, not the norm. And when they do happen,
they can be managed through effective treatments such as antihistamines or epinephrine.
And, there are things that
you can do to help prevent food allergies in your child. Our goal at
First Bites is to empower you with the knowledge and tools to face food allergies with increased confidence and support.
Food Allergies vs. Food Intolerances
Food allergies are different from food intolerances.
Food allergies involve the immune system and can be serious or life-threatening. In contrast, food intolerances primarily involve the digestive system and do not involve the immune system. We compare and contrast these two types of food reactions below:
Caused by immune system reactions to a specific ingredient
Caused by the digestive system being unable to break down a food
Even tiny amounts of the food can set off a reaction
May not result in symptoms if only a small amount of food is eaten
Can affect multiple body systems (e.g., breathing or respiratory system, skin, digestive system, etc.)
Does not affect bodily systems besides the digestive system
Reactions are rapid, usually occurring within two hours of ingestion
Symptoms appear a few hours after consumption, as the food makes its way through the digestive system
Can result in life-threatening symptoms
Causes discomfort (e.g., stomach pain, bloating) but is not life-threatening
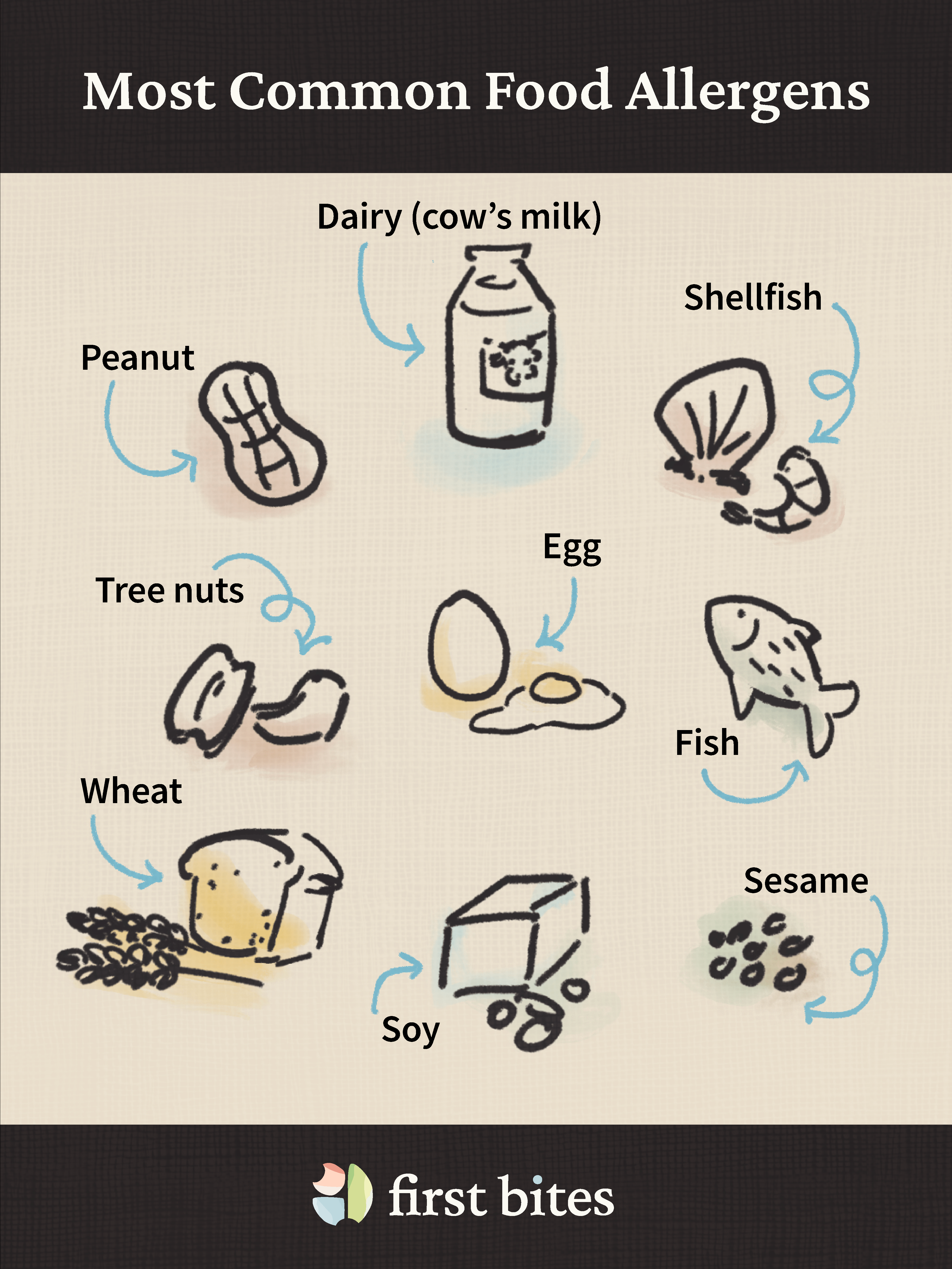
The Big 9: The Most Common Food Allergens
While any food can potentially cause allergies, these nine food groups account for about 90% of food-based allergic reactions:
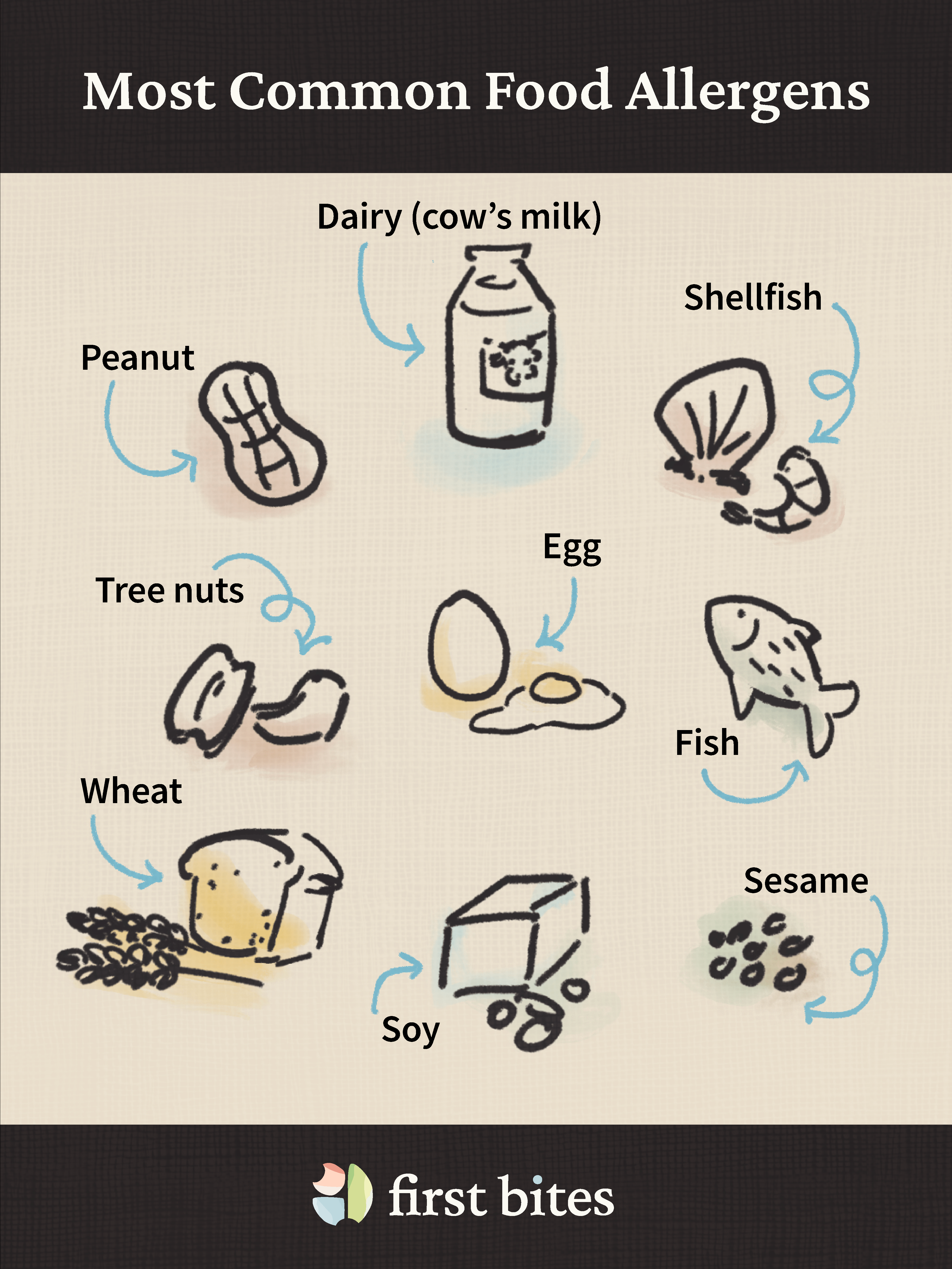
- Dairy (cow's milk)
- Eggs
- Fish (finned fish like salmon, tuna, etc.)
- Shellfish (shrimp, crab, etc.)
- Tree nuts (almonds, cashews, walnuts, pistachios, pecans, hazelnuts, pine nuts, and Brazil nuts)
- Peanuts (a legume, not a tree nut)
- Wheat
- Soy
- Sesame
Some other common allergens seen in children include sunflower seeds and other legumes such as chickpeas, green peas, and lentils.
Risk Factors for Food Allergies
Human bodies are complex, making it difficult to point to any single cause or simple explanation for why some babies, but not others, develop food allergies. It is important to emphasize: Any baby can develop food allergies, and sometimes we just don’t know exactly why.
That being said, certain factors have been found to suggest a higher risk for developing food allergies:
- Eczema is the strongest known risk factor. Babies with eczema are significantly more likely to develop food allergies. The more severe the eczema, the higher the risk of food allergies. So, babies with moderate to severe eczema are at higher risk than those with mild eczema, but babies with mild eczema are still at higher risk than babies without eczema.
- Existing food allergies are also strongly linked to higher risk of developing additional food allergies. In other words, if your baby is diagnosed with an allergy to one food, they are likely allergic to other foods as well.
- Delayed allergen introduction may also increase the risk of developing food allergies. Current guidelines recommend beginning introduction of the most common food allergens around 4-6 months, or just after your baby begins eating solid foods, as a way to prevent food allergies.
- Family history of allergic diseases, including food allergies, asthma, eczema, and hay fever, may increase the risk of developing food allergies. The risk associated with family history of allergic diseases is not as strong as the other risk factors listed here, such as eczema. However, if such a family history does exist for your baby, it could be worth bringing it up with your pediatrician.
Keep in mind that
for all babies, early and regular exposure to common food allergens can reduce the risk of developing food allergies. In fact, early introduction may be extra impactful for babies with any of the above risk factors given their heightened baseline risk for developing food allergies. Recommended allergen exposure schedules as well as helpful tips for introducing allergens and a user-friendly food tracker are included in the
First Bites app to help with the process.
Eczema is the #1 Risk Factor for Food Allergies
Active involvement in preventing food allergies is even more important for babies with eczema than for babies without eczema.
This is because moderate to severe eczema is the strongest known risk factor for developing food allergies. Eczema is a common condition that causes dry, itchy skin and is linked to a weakened skin barrier. A strong skin barrier protects your body from outside elements and helps retain moisture. A weakened skin barrier means that outside elements, such as food allergens, can make their way into the body through the skin — even if the food is not consumed. This, in turn, can increase the likelihood that the immune system identifies these as intruders (i.e., sensitization).
If your baby has eczema, managing the skin condition is one of the best ways to reduce food allergy risk. In fact, it is critical to have the eczema under control before introducing food allergens altogether. It’s best to work with your pediatrician to develop a treatment plan. This may include daily moisturizing with fragrance-free moisturizers, which can help maintain your baby’s skin barrier, or prescription treatments for the inflammation.
For babies with eczema, regular exposure to food allergens can be even more beneficial for allergy prevention given their higher baseline risk. In other words, eczema makes early introduction even more important, not less. Also, food allergens do not cause eczema. So, as long as the eczema is being managed, allergen exposure only holds benefits for prevention without any downsides.
The takeaway: If your baby has eczema, they are at higher risk for developing food allergies, which makes everything you do for prevention potentially even more impactful.
Allergen Introduction
Why Introduce Allergens Early?
Guidelines for allergen exposure have changed in the past decade. The most up-to-date guidance from the American Academy of Allergy, Asthma & Immunology states that it is not only safe, but actually recommended to introduce allergens soon after your baby starts solids — that is, around 6 months old but not before 4 months, and after your baby has already tolerated some common starter solids.
There is strong evidence that early introduction of peanut and egg can reduce the risk that your baby becomes allergic to these foods. While the evidence for other allergens is not as strong, there is no evidence against including all of these foods in your baby’s diet early on.
How to Introduce Allergens Safely
Before You Start
- Make sure your baby is developmentally ready for solids (for instance, good head and neck control, and showing interest in foods).
- Try a few non-allergenic foods first, and make sure that your baby tolerates them well.
- Plan to introduce allergens during daytime meals rather than at night, so you can monitor for reactions.
- Have your pediatrician's contact information handy, so you can reach out for more guidance in case your baby has a reaction to the food.
The Step-by-Step Process
- Start small: Begin with just 1/8 to 1/4 teaspoon of the allergenic food. Keeping the quantity small means that even if your baby does have a reaction, the reaction is more likely to be mild and manageable at home.
- Wait and watch: Observe your baby for about 10 minutes after the first taste.
- Offer more: If no reaction occurs, offer a bit more during the same meal.
- Continue regular exposure: Contrary to what you might think, this is not a “one and done” process.
And finally, just like any other food,
introduce allergens in developmentally-appropriate ways. For example, thin nut butters with formula, breast milk, or water to minimize choking concerns when introducing tree nuts. Alternatively, include nut powders in your favorite baby-safe recipes. Avoid whole nuts, large chunks, and sticky nut butters because they pose choking hazards.
Remember, this is not a "one and done" process. Regularly offering tolerated allergens throughout childhood is needed to maintain the protective effect and reduce the risk of developing future allergies. For more guidance,
here are some doctor-backed recommendations we have put together on how often to serve each allergen, as well as suggestions for how to serve them. And if you need help staying on top of keeping regular exposure going, we can help with the
First Bites app.
Unfortunately, regular exposure cannot guarantee prevention of all food allergies. Some children will be diagnosed with food allergies despite early introduction efforts. Not everything is under our control, and many factors can contribute to the development of food allergies in children that are not yet fully understood. If this happens, please remember to pat yourself on the back for doing everything you can for your child! And, when you’re ready, we have put together more information about
what to do if your child is diagnosed with a food allergy.
Why You Should Document Your Baby's Food Journey
There’s more than enough to keep track of as a parent, from when you last did laundry to where you last saw your baby’s favorite toy. It can be overwhelming to consider adding even more to the list — especially something as constant and unending as what your baby eats.
Yet, keeping track of what your baby is eating can be a key component of identifying and preventing food allergies. This is because the process of narrowing down the cause of a food reaction and identifying next steps relies on knowing a whole host of factors, including:
- What your baby ate, how much, when, and with what other foods;
- Whether and when they had eaten that food before;
- What reaction they had, if any;
- Whether they had previously reacted to that food;
- And more...
Keeping track of this information using a tool like the
First Bites app will help you and your pediatrician
identify patterns that are otherwise easily missed,
assess concerning symptoms in the context of your daily life, and
ensure consistent allergen exposure to maximize the preventive benefits of early exposure.
Documenting your baby’s food journey is important, but it doesn’t have to be hard. First Bites was designed to take the mental load off parents while ensuring babies get the consistent allergen exposure they need for ongoing protection as they age.
Questions to Ask Your Doctor
Your regular pediatric check-up appointment is a great time to bring up allergen introduction and receive medical advice specific to your child. Allergen introduction can be discussed at the same appointment that you talk about starting solids (when your baby is around 4-6 months).
Below, we’ve included several useful questions to help you get the conversation started. These questions can help every family as they navigate their child's food journey. However, if your baby has
certain risk factors, such as severe eczema, existing allergies, or family history of food allergies, it can be especially important to talk to your pediatrician about introducing allergens sooner rather than later.
Before Starting Allergen Introduction
- "My baby has eczema. What special precautions should I take when introducing allergens?"
- "What is the right Children's Zyrtec dose for my baby's weight?"
- "Are there any specific foods we need to introduce in clinic given our family history?"
During the Introduction Process
- "I think my baby had a mild reaction to [this food]. How can I tell if it was an allergy or just contact irritation?"
- "My baby refuses certain allergens. What are some other ways to offer them?"
- "Should I be concerned about how much my baby is eating of each allergen?"
- “Are there any allergens we should wait to introduce in clinic?”
If Reactions Occur
- "My baby had hives after eating [this food]. What should I do next?"
- "How can we confirm whether or not this was a true food allergy?"
- "When is it safe to try the food again, and should it be done at home or with a physician?"
Potential Reactions
How to Recognize Allergic Reactions
There is a range of possible allergic reactions that your child could experience. The symptoms listed below can appear on their own or in combination, and will appear within minutes to two hours after eating.
The majority of reactions during early allergen introduction are mild and manageable at home, especially if the quantity consumed is small.
Severe reactions, such as anaphylaxis, are rare and can usually be avoided by following
these doctor-backed recommendations for allergen introduction.
Common allergic reactions fall into the categories of
skin symptoms, digestive symptoms, or
respiratory symptoms:- Skin symptoms include hives (raised, red, itchy bumps that can appear anywhere on the body), swelling (especially of face, lips, or tongue), flushing, or widespread redness. For babies, the most common reactions you will see are in this category.
- Digestive symptoms include persistent vomiting (more than normal spit up), diarrhea, unusual fussiness, or signs of stomach pain.
- Nasal symptoms include runny nose, congestion, or sneezing.
- Respiratory symptoms include wheezing, cough, and shortness of breath.
If you see any of these symptoms in your baby, contact your pediatrician for further guidance. It will be particularly important to reach out if you observe hives or widespread rash, vomiting, swelling (face, lips, or tongue), or significant behavior changes. For skin symptoms, a good strategy is to take a picture and send it to your pediatrician to help assess severity.
Anaphylaxis is a rare but serious and potentially life-threatening allergic reaction. If you suspect anaphylaxis, call 911 immediately. Symptoms include:
- Difficulty breathing, wheezing, or severe cough
- Swelling of throat or tongue
- Severe whole-body hives
- Vomiting or diarrhea combined with other symptoms
- Light-headedness or fainting, dizziness, or confusion
- Loss of consciousness or extreme drowsiness
- Pale or blue coloring, especially around lips
Knowing the symptoms of an allergic reaction means you are better prepared to respond if the need arises. It also means you know what to
look for and record to identify potential trigger foods with your child’s doctor.
Contact Irritation vs. Food Allergy
Many babies, especially those with sensitive skin, develop redness or a mild rash around their mouth when eating certain foods. This is often contact irritation, not an allergic reaction.
Limited to where food touched the skin (around mouth, chin, hands)
Mild redness or rash
No other symptoms
Symptoms beyond the contact area
Can affect multiple body systems
Can result in severe rash or hives
Appears rapidly and resolves quickly when food is wiped away
Symptoms appear within two hours of eating
Symptoms may persist or worsen over time
Caused by foods that irritate sensitive skin (e.g., acidic foods, spiced foods)
Mostly caused by the most common food allergens (e.g., tree nuts)
Contact irritation can be caused by foods that may irritate sensitive skin. Common irritants include acidic foods like tomatoes, oranges and citrus, and strawberries or spiced foods such as those with cinnamon, cloves, coriander, fenugreek, and garlic.
Contact irritation is not dangerous. Children can continue to eat the foods that caused the irritation, and irritation often improves with repeated exposure. If your child experiences contact irritation, gently wipe their face during and after eating. If their skin is sensitive overall, some common brands of wet wipes can cause irritation. Instead, try wetting a soft dry wipe with water to reduce potential irritants to the skin. Prior to offering the food, it can also be helpful to put petroleum jelly (Vaseline) or an unscented moisturizer around your baby’s mouth, chin, and hands (especially if they are eating with their hands) to provide a protective barrier on your baby’s skin.
FPIES: A Different Type of Food Allergy
Your baby could have a reaction to a food that is not an IgE-mediated food allergy (which is the most common type). The reaction could be the result of contact irritation, which is not dangerous and should not prevent you from continuing to offer the food. It could also be Food Protein-Induced Enterocolitis Syndrome (FPIES) — another type of food allergy which can be concerning and requires medical diagnosis and attention.
FPIES is a non-IgE-mediated food allergy — in other words, it is caused by other parts of the immune system (T-cells and white blood cells). FPIES cannot be treated with antihistamines or epinephrine. Other differences include:
- Onset: FPIES symptoms appear later than an IgE-mediated allergic reaction. FPIES symptoms appear anywhere from 1-4 hours, or up to 10 hours, after food exposure. An IgE-mediated food allergy reaction, by contrast, appears soon after exposure.
- Symptoms: FPIES symptoms primarily involve repetitive, severe vomiting (1-4 hours after eating) and diarrhea (5-10 hours after eating). Additional symptoms include extreme fussiness or lethargy, pale skin color, and dehydration. FPIES does not result in hives or breathing problems, unlike food allergies.
- Triggers: FPIES is more commonly triggered by foods such as cow’s milk, soy, rice, oats, and some vegetables like sweet potato and avocado. This is different from the most common food allergens, though there is some overlap with cow’s milk, soy, eggs, and peanut.
- Treatment: FPIES treatment focuses on avoiding trigger foods. Common treatments such as antihistamines and epinephrine will not help.
If you suspect FPIES, contact your pediatrician immediately. This condition requires medical diagnosis and management.
Be Ready In Case of Reaction: Have a Plan
For most babies, trying common allergens is both safe and recommended to prevent developing future allergies. However, it remains possible that your baby may react to a food. No need to panic — being prepared and knowing what to do if needed will help you navigate the situation.
1. Prepare an Emergency Kit
Before introducing a new allergen, it is helpful to prepare an “emergency kit” with useful items in case of a reaction. These include:
- Children's Zyrtec (cetirizine): Liquid Children's Zyrtec can help treat mild allergic reactions, such as hives or itching. Symptoms should subside or improve approximately 15 minutes after treatment. You can find general dosing guidelines here, but confirm the appropriate dose with your pediatrician or pediatric allergist.
6-11 months (12-17 lbs)
2.5 mL once daily
12-23 months (18-23 lbs)
2.5 mL once daily, can increase to twice daily if needed
2-5 years (24+ lbs)
2.5 to 5 mL once daily, can increase to twice daily if needed
- Epinephrine: Children with one diagnosed food allergy are at higher risk for other allergies. When introducing a new allergen to a child with a diagnosed food allergy, it is critical to have your epinephrine (Epi-Pen or Neffy, which is a nasal spray form of epinephrine) nearby. Use your epinephrine immediately if your child is showing signs of anaphylaxis.
- Emergency contacts: Having the phone numbers for your pediatrician’s office as well as local emergency services can help you save time in a stress-inducing situation.
2. What to Do in Case of an Allergic Reaction
Now that you have your emergency kit, you’re ready to introduce your child to the allergen. Stay alert for any signs of allergic reaction and be ready to act if needed:

- Hives, mild swelling, or itching

- Mild upset stomach
- Occasional spitting up
- Take a picture and send it to your pediatrician, or call for immediate guidance
- Treat with antihistamines (Children's Zyrtec)
- Monitor closely

- Hives
- Facial swelling
- Widespread redness or flushing
- Persistent congestion
- Mild cough

- Persistent vomiting
- Cramping
- Diarrhea
- Treat with antihistamines ( Children's Zyrtec)
- Call your pediatrician

- Hives across the whole body
- Significant swelling of the face, lips, and/or tongue
- Swelling in other parts of the body
- Difficulty breathing
- Wheezing
- Severe Cough

- Vomiting and diarrhea AND other symptoms
- Pain in the stomach with severe cramping
- Dizziness
- Confusion
- Fainting or loss of consciousness
- Call 9-1-1 immediately
- Use epinephrine if you have it
Anaphylaxis is a serious, life-threatening condition that requires immediate medical attention. Be particularly vigilant if you see any of the following symptoms of anaphylaxis:
- Difficulty breathing, wheezing, or severe cough
- Swelling of throat or tongue
- Severe whole-body hives
- Vomiting or diarrhea combined with other symptoms
- Rapid pulse, dizziness, or confusion
- Loss of consciousness or extreme drowsiness
- Pale or blue coloring, especially around lips
3. After the Reaction
The first time your baby has a reaction to food can be scary. After ensuring your child has received the care they need, be sure to take time to recognize all that you are doing and have done for your child!
Because reactions can be the result of many factors and may not necessarily mean a food allergy, the next step is to confirm the diagnosis of a food allergy with a doctor. Work with your pediatrician or pediatric allergist through this process. Receiving a food allergy diagnosis opens up a whole new set of demands. If you find yourself in this situation, we’ve created another guide for
what to do when your child is diagnosed with a food allergy. Remember, you’re not alone.
The Bottom Line: You're Helping Prevent Allergies
Now that you’ve made it this far, it’s time to pat yourself on the back and acknowledge the care and attention you are providing to your child! We’ve included a lot of information in this resource article, so please give yourself time to slowly digest it all. In the meantime, here are some bottom-line takeaways for you to hold onto:
Your actions can help prevent food allergies in your baby. By introducing allergens early and consistently, you are actively working to prevent potential food allergies.
Early introduction of allergens is beneficial for all babies. The protective effect of early introduction applies regardless of whether your baby is high-risk or not. The research is clear and consistent: Babies who receive early, regular exposure to allergens have significantly lower rates of food allergies later in life.
Most babies will not have reactions to food, and those who do usually experience mild and manageable symptoms. Keep in mind that the vast majority of babies tolerate allergen introduction without any problems, and that introducing small amounts to start with means that any reactions tend to be mild.
Trust yourself, and trust the process. There is strong evidence supporting early allergen introduction to prevent food allergies. Even if the journey feels long, know that you are following the best science to give your baby the best chance at a life free from food allergies.
You are doing a great job! The only universal truth in parenting is to expect the unexpected. Every baby is different: Some babies will need multiple exposures before accepting new foods. Some will have mild contact irritation. Some will refuse certain textures. All of this is normal. Remind yourself that you are doing what you can, and what you are doing matters greatly for the overall well-being of your child.
Try and find time to enjoy the small moments. In the end, we are all motivated by love for our children and the desire to provide them with the best life possible. So, don’t forget to enjoy the time with your baby, even if they are spitting out your carefully prepared peanut recipe — just keep trying! No matter how the journey looks for you and your family, and no matter how you’re feeling at any given moment, we’re here to remind you: You’re doing amazing.
Here’s to the many varied, nutritious meals you and your family will enjoy in the coming years!